LED implant offers new hope in cancer treatment
Advancements in medical technology continue to push the boundaries of cancer treatment, and a recent innovation in photodynamic therapy (PDT) could mark a significant breakthrough.
Researchers at the University of Notre Dame have developed a miniature wireless LED device designed to induce cell death in cancerous tissues through a process called pyroptosis. This new technology offers the potential for treating deep-seated tumours with greater precision and fewer side effects compared to conventional methods.
The challenge of light penetration in PDT
Photodynamic therapy relies on the use of light to activate a photosensitiser dye that produces reactive oxygen species (ROS) to kill cancer cells. However, the limited penetration of visible light through biological tissues has restricted PDT primarily to surface-level treatments. This limitation has driven the need for innovative solutions to deliver light effectively to deeper tissue sites.
The miniature wireless LED device
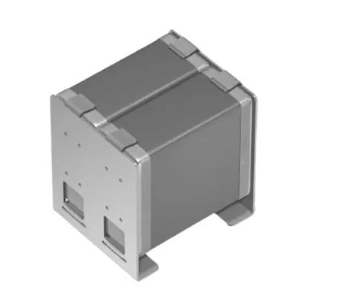
The research team, led by Sunghoon Rho and colleagues, has addressed this challenge by creating a miniature LED device with a volume of just 23mm³. This device is powered wirelessly by radiofrequency (RF) energy, allowing it to emit light at a wavelength of 573nm. This specific wavelength is optimal for activating Rose Bengal, a green-absorbing dye known for its efficiency in producing type II photosensitisers.
The device's wireless power transfer capability has been demonstrated effectively even when buried in chicken breast tissue, up to a depth of 6cm from the transmitting antenna. This feature highlights its potential for deep-tissue applications, overcoming one of the significant barriers in current PDT techniques.
Inducing pyroptosis
One of the remarkable findings from the study is the device's ability to induce cell pyroptosis in cultured HT-29 human colorectal adenocarcinoma cells. Pyroptosis is a form of programmed cell death that is highly immunogenic, meaning it can stimulate an immune response against the tumour. This process was evidenced by the time-dependent generation of bubbles in the photoactivated cells and further confirmed through cell staining techniques.
The LED device, in combination with Rose Bengal, successfully photogenerated enough singlet oxygen to cause significant cell death, with a notable increase in cell inactivation observed with prolonged light exposure. This approach not only kills cancer cells directly but also has the potential to convert an immune-silent tumour into an immunogenic one, enhancing the body's ability to fight cancer.
Practical applications and future directions
The miniature LED device represents a significant step forward in the field of PDT. Its small size allows for less invasive implantation methods, and its wireless power capability means it could be programmed for extended treatment periods, offering a practical solution for both preclinical and clinical applications.
Future research aims to explore the use of longer-wavelength photosensitisers that can penetrate deeper into tissues, further expanding the potential applications of this technology. Additionally, combining the LED device with drug release technologies could create multifunctional therapeutic tools capable of real-time feedback and controlled treatment delivery.
The development of this miniature wireless LED device opens new avenues for cancer treatment, particularly for deep-seated tumours that have been challenging to treat with traditional PDT methods. By harnessing the power of light-induced pyroptosis, this technology has the potential to change the way cancer therapy is approached, making treatments more effective and less invasive. As research continues, the future of photodynamic therapy looks brighter than ever.