Needle simulator aims to revolutionise medical training
Administering needle-based procedures in anesthesiology, such as epidurals, is a complex and delicate procedure and the current training methods for doctors are costly and fall short in preparing them for every patient and situation they will face. A new provisional patent from the Penn State College of Engineering plans to change that.
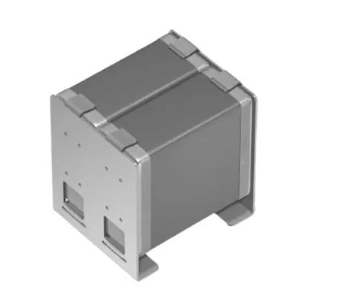
The haptic-force needle-insertion simulator, created by a team of researchers led by Jason Moore, associate professor of mechanical engineering, is a low-cost, hand-held device that simulates the tactic feeling of the instrument passing through several layers of tissue. It also connects to a computer program that can assess the user’s performance.
These factors are crucial because the doctor’s hands need to produce a steady rate of insertion, which can be challenging. “There’s a buildup of force upon tissue deflection and a sudden release of force upon tissue puncture,” Moore said. “This training tool can help surgeons, residents and med students improve their dexterous abilities.”
Working in harmony, the tool and program interface will provide real-time feedback on the physician’s performance during training. This response is crucial to the device and represents a new efficiency and effectiveness of surgical training. Currently, the most effective way to train clinicians is to observe other doctors.
“Those of us who teach these procedures find it very difficult to teach the needle, eye and image coordination skills,” said Sanjib Adhikary, associate professor of anesthesiology, Penn State Hershey and co-investigator of the project. Using the simulator, doctors will be better prepared for these procedures.
“It can raise the ability of residents before they begin performing these procedures on patients,” Moore said. “It also gives them a very nice way to assess their performance and understand where improvements can be made.”
Other training methods, like using mannequins, are more expensive and do not account for the range of body types a doctor would encounter in their patients. This device is able to change its simulation based on these different scenarios, like varying skin thickness and excess body weight.
“Being unprepared for diverse patient scenarios can increase the probability of complications occurring, and this training will help the doctor’s ability to adapt,” Moore said. Eventually, this tool could be adapted to train doctors in other specialties like emergency medicine, radiology and surgery.
“This project has the potential to revolutionise training on surgical procedures,” said Scarlett Miller, associate professor of engineering design and industrial engineering, Penn State. The rest of the team is also confident their device will make an impact, especially as it represents a low-cost method to this common problem.
“We’re really excited because the device is slated be relatively low cost, less than $100,” Moore said. “I would love to see this widely applied, all the way down to undergraduate pre-med programs. It could be impactful to easily assess this skill and provide meaningful feedback to allow for continuous improvement.”
Moore, Adhikary and Miller recently received an ENGINE grant from the College of Engineering to commercialise the product. “This grant has really accelerated our work,” Moore said.
The team hopes to test the device at Penn State Hershey and receive feedback from physicians next fall. “This project is in its infancy, but we hope it could follow the [central venous catheter] robot we worked on that is now a part of the surgical residency training curriculum at Hershey Medical Center,” Moore said.
Miller added, “This project not only has the potential for commercial value, but also for helping save human lives.”