Would you trust a robot to perform hip surgery on you?
Sam Holland looks at an extensive study, called RACER-Hip, that compares the performance of traditional surgery with robot-assisted surgery, and considers how comfortable people may be with the latter.
What does robot-assisted hip surgery entail?
As covered on Electronic Specifier in the past, the use of robots in hospitals, such as that seen in remote-controlled robotics, is becoming more and more common. And there are many reasons for this, such as the need to reduce the fatigue of hospital staff who would otherwise need to travel long distances throughout the hospital to perform patient care. In the case of robot-assisted hip surgery, such surgery is performed by a robotic arm but remains similar to traditional hip surgery.
This is as much of the process still requires a human surgeon to manually remove a patient’s damaged tissue. The difference is where the artificial replacement comes in: rather than having the artificial joint installed by the surgeon, it is the job of a dedicated robotic arm to make the incision and administer the implant.
The main query that arises, namely, ‘Would you trust a robot to perform hip surgery on you?’, reflects one major concern that arises in all areas of automation (not just those relevant to medical robotics): the question of how well the technology performs compared to its human counterpart(s).
Putting it to the test
The question of how machines compare to human surgeons is what a university study named RACER-Hip is aiming to solve. Standing for ‘Randomised controlled trial for Hips’, RACER-Hip (also see RACER-knee for its knee replacement equivalent) has been provided £1 million in funding by NIHR – the National Institute for Health and Care Research. It is being run jointly by the University of Warwick’s Warwick Medical School, UHCW (University Hospitals Coventry and Warwickshire) NHS Trust, and the Royal Orthopaedic Hospital in Birmingham.
The long-term study will see all participants being placed in two equally-populated treatment groups: one that will receive hip replacements from a human (the control group), and the other one from a robot (the experimental group). Aside from observing the initial surgery quality, the research will collate the answers to participants’ questions, such as those regarding each patient’s ease of movement and quality of life, particularly in the long run.
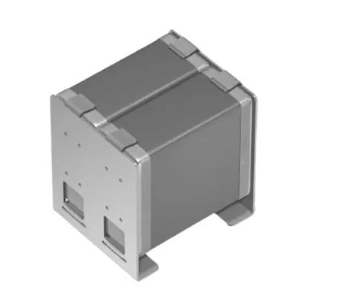
Stryker’s robot for RACER-Hip’s study into the comparison between the performances of human-only and robot-assisted hip replacement surgery. Image credit: Stryker
The research is a much-needed extensive study into the benefits of adding more automation to hospital procedures. And according to NIHR, Stryker, the manufacturer of the above-pictured surgery robot for RACER-Hip, will even pay for the costs of any further hospitals that wish to take part in the research.
Considering the prospective findings
As mentioned above, the question that spans almost all areas of automation must be addressed: how well does technology perform when compared to its human counterpart(s)?
At the time of writing, it will require speculation to consider what will be seen in the findings of the currently far-from-complete RACER-Hip study (the news broke on the 8th of July, 2022). However, there are three key points that invite some educated guessing:
-
The human-only surgery on the control group is to be carried out just as safely and accurately as it would have been even if no such study existed.
-
The robot-assisted surgery on the experimental group will be a product of a leading medical robotics company – and even then, the operation may be overseen by an additional human surgeon and/or representative of the manufacturer.
-
Even if no such additional human supervisors are present throughout the robot-assisted surgery, the operation will still be exactly that: robot-assisted. The whole study will always require human surgeons. There are no participants who will receive solely robot-based surgery.
All of this means that there will never be a time when the robot will be left alone in any operations. So what RACER-Hip’s findings will likely go on to clarify is this: the talents and dexterity of human surgeons become even better when their procedures are robot-assisted. This will be made especially clear if or when the findings reveal that the participants who underwent robot-assisted surgery went on to have the following benefits: more ease of movement, better quality of life, and a more seamless incision and, therefore, less post-surgical pains.
And that third and final point is especially crucial, because it draws on the question of how precise traditional surgeries are when compared to their robotic-assisted equivalents. After all, there is no such thing as a truly ‘steady hand’, but there is such a thing as a ‘dead still’ robotic arm. Therefore, while human skills remain vital, the limitations that arise from the imperfect dexterity of human surgeons’ hands (which can, and likely should, be complemented by a robotic arm) must also be taken into consideration.
In fact, perhaps the term ‘robot-assisted surgery’ should be called ‘robot-enhanced surgery’. This would indicate that the thinking and management behind the surgery remains human-led, while also reflecting that the robot is used more as a tool (rather than any kind of ‘assistant’ as such): one that sees the surgeons’ capabilities, not just supported – but rendered better still.
Would you trust a robot to perform hip surgery on you?
Perhaps people's current concerns shouldn’t so much be about robot-assisted surgery as we know it today – but the question of where the technology will go from here. There are already legal complications that arise from any use of any robot in any form of surgery. But concerns over patient health and safety will become immensely more complicated if or when surgical robots become increasingly trusted outside of human supervision and control.
On top of this, many people have technophobia (also consider automatonophobia which encompasses a fear of human-like robots), which all the robot engineering in the world may never resolve. This makes the importance of patient discretion all the more marked, and this is reflected by the fact that the RACER-Hip study was completely optional: it only put patients in the position of being randomly selected for robot-assisted surgery if they had opted in to it in the first place.
With all the above considerations in mind, perhaps, most people's answer to the question, ‘Would you trust a robot to perform hip surgery on you?’, will sound something like this:
‘Only if I were given the choice whether I wanted to opt in, along with plenty of time to opt out if I change my mind. And the robot must also be accompanied by as many human surgeons as possible, right there in the operating theatre – pulling the strings at all times.’