Mini rolling robot takes virtual biopsies
Researchers have developed a tiny magnetic robot which can take 3D scans from deep within the body and could revolutionise early cancer detection.
The team say this is the first time it has been possible to generate high-resolution three-dimensional (3D) ultrasound images taken from a probe deep inside the gastrointestinal tract, or gut.
It paves the way to a transformation of the diagnosis and treatment of several forms of cancer by enabling ‘virtual biopsies’, non-invasive scans that provide immediate diagnostic data.
This will allow doctors to detect, stage, and potentially treat lesions in a single procedure, eliminating the need for physical biopsies.
Delivering immediate results
Pietro Valdastri, Professor and Chair in Robotics and Autonomous Systems and Director of the Science and Technologies of Robotics in Medicine (STORM) Lab and who coordinated the research behind this paper, said: “For the first time, this research enables us to reconstruct a 3D ultrasound image taken from a probe deep inside the gut – something that has never been done before.
“This approach enables in-situ tissue analysis and diagnosis of colorectal cancer, with immediate results.
“The process of diagnosing colorectal cancer currently requires a tissue sample to be removed, then sent to a lab, with results taking from one to three weeks.”
Unique rolling motion
The perhaps surprising key to the team’s success was the use of a little-known 3D shape, the oloid.
This gave the magnetic medical robot a previously impossible range of motion, the roll, essential for precise navigation and imaging inside the body.
A paper, published 26 March 2025 in Science Robotics, explains how the team integrated the oloid shape, and its unique rolling motion, into a new magnetic flexible endoscope.
They equipped it with a small, high-frequency imaging device to capture detailed 3D images of internal tissues.
The imaging device, a 28 megahertz micro-ultrasound array, creates a high-resolution, 3D reconstruction of the area it scans.
Virtual reconstruction
From this virtual reconstruction, clinicians can make cross-sectional images that mimic those generated by a standard biopsy.
During a standard biopsy, a sample of tissue is sliced into thin layers and placed on a slide to be examined under a microscope.
High frequency, or high-resolution ultrasound, is different to the ultrasound most of us are familiar with, used to look at a foetus or internal organs.
The high frequency and resolution ultrasound probe used in this study enables users to see features on a microscopic level, down to tissue layer level detail.
While 3D ultrasound can already be performed in blood vessels and in the rectum, this work opens the possibility for 3D scans to be performed deeper in the gastrointestinal tract.
Cutting-edge technology
Jane Nicholson, Executive Director of Research at EPSRC, said: “Progress from cutting-edge technology developments is enabling the development of rapid, non-invasive solutions that have the potential to revolutionise cancer diagnosis and treatment.
“By improving the precision and control of procedures for high-incidence cancers such as colorectal cancer, the efforts of this interdisciplinary team could lead to significant advancements in cancer detection and treatment.”
Improving patient outcomes
Postgraduate researcher Nikita Greenidge, a member of Leeds’s STORM Lab, in the School of Electronic and Electrical Engineering, and lead author of the paper, said: “By combining our advanced robotics with medical ultrasound imaging, we take this innovation one step ahead of traditional colonoscopy, allowing doctors to diagnose and treat in a single procedure – eliminating the wait between diagnosis and intervention.
“This not only makes the process more comfortable for patients but also reduces waiting times, minimises repeat procedures, and alleviates the anxiety of waiting for potential cancer results.
“Colorectal cancer is one of the leading causes of cancer-related deaths in the UK and globally, but if detected early it is highly treatable.
“This research presents a new approach that could significantly improve early diagnosis with a minimally invasive approach and could also, in future, facilitate targeted ultrasound-triggered drug delivery for more effective treatment.”
Testing the approach
The research found that using the oloid, a shape formed by two intersecting perpendicular circles, significantly enhanced the dexterity, diagnostic capabilities and autonomy of magnetic flexible endoscopes, and magnetic medical robots overall.
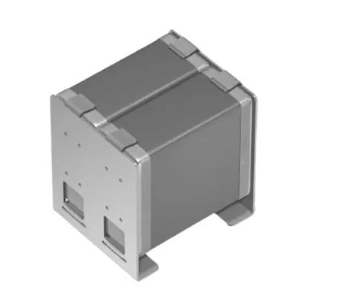
The oloid magnetic endoscope (OME) was 3D printed out of resin, measuring just 21mm in diameter, around the size of a 1p coin.
This meant that the robot could still roll but was a practical size and design for clinical applications like colonoscopy.
Its movement was tested on a range of surfaces simulating the structures of the colon, oesophagus and stomach.
The results
To advance the technology toward human trials, the team first conducted tests in an artificial colon, followed by studies in pigs, a necessary step in meeting regulatory requirements for medical device approval.
They used a robotically controlled external permanent magnet, a platform previously developed at Leeds which enables both joystick and autonomous control of the OME.
Navigation was assisted by images from an embedded camera and a magnetic localisation system.
The results demonstrated that the system could:
- successfully perform controlled rolling and sweeping motions inside the colon
- generate high-resolution 3D ultrasound scans for accurate diagnosis
- identify lesions in gastrointestinal tissue, showcasing its potential for advanced medical imaging and early disease detection
Further opportunities
While this research had been conducted in the colon, the rolling properties of the oloid shape could be applied to a variety of magnetic medical robots.
This could potentially expand its applications to other areas of the body.
The team will now set about collecting all the data that will allow them to conduct human trials, which they hope could start in 2026.
This technology was developed through a collaboration between engineers, scientists and clinicians from University of Leeds, University of Glasgow, The University of Edinburgh. The technology was funded by: Engineering and Physical Sciences Research Council (EPSRC), European Commission, European Research Council, National Institute for Health and Care Research Leeds Biomedical Research Centre.