World's first patient leaves hospital with titanium artificial heart
An Australian man in his forties has made history by becoming the first person in the world to leave the hospital with a titanium-based artificial heart.
This pioneering device, designed as a temporary solution for individuals suffering from heart failure while awaiting a heart transplant, had previously only been used in patients who remained in hospital under constant medical supervision.
The patient, who had the BiVACOR artificial heart implanted, lived with the device for over three months before undergoing a successful heart transplant surgery. He is now recovering well, according to a statement released by St Vincent’s Hospital in Sydney, Australia, where both procedures took place. This makes him the sixth individual worldwide to receive the BiVACOR heart, but the first to live with it for an extended period of time, surpassing the one-month threshold previously recorded.
Julian Smith, a cardiac surgeon at the Victorian Heart Institute at Monash University in Melbourne, commented on the significance of the achievement, saying: “This is certainly an important development in the field.”
Who is BiVACOR?
BiVACOR is an Australian-based medical device company focused on developing innovative heart replacement technology for individuals suffering from end-stage heart failure. The company was founded with the mission to address the challenges posed by heart failure and the shortage of donor organs.
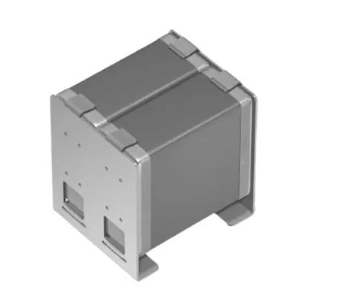
Its flagship product is the BiVACOR artificial heart, invented by biomedical engineer Daniel Timms, which aims to be a long-term, life-saving solution for patients who require a heart transplant but either cannot get one due to organ shortages or are not candidates for existing mechanical assist devices.
The technology
The BiVACOR artificial heart features a centrifugal pump design, which allows for continuous blood flow, mimicking the natural pumping action of a healthy heart. Unlike traditional heart pumps that rely on multiple components and complex mechanisms, the BiVACOR heart uses a single moving part, a rotor, which simplifies the device's design and improves its durability.
The rotor is made from biocompatible materials to ensure it can safely remain in the body for extended periods. This design reduces wear and tear compared to existing mechanical heart pumps, potentially extending the device's lifespan far beyond what is currently achievable with other options. By relying on one moving part, the BiVACOR heart offers a more mechanically robust solution for patients.
One of the key features of the BiVACOR heart is its continuous-flow technology. This means the device keeps blood moving smoothly without the pulsatile action seen in the natural heart. While this differs from how the human heart typically functions, continuous-flow pumps have proven effective in similar medical devices, such as Left Ventricular Assist Devices (LVADs).
Another advantage of the BiVACOR device is its long-term durability. With fewer moving parts and a simpler design, the device is expected to last longer than conventional heart pumps, which often require replacement every 5-7 years. This durability could be especially beneficial for patients who require a long-term solution to heart failure.
Additionally, the BiVACOR heart is designed to be fully implantable, meaning that all components are contained within the body, eliminating the need for external equipment. This makes the device more streamlined and potentially less invasive than current heart-assist devices, which often require external pumps or wires.
The device’s biocompatibility is another crucial feature, as it reduces the risk of complications such as blood clots, which are common with other heart pump devices. This biocompatibility ensures that the BiVACOR heart can remain safely inside the body without causing adverse reactions, increasing its potential for long-term use.
Unlimited potential
Despite the milestone, there are still many challenges and uncertainties surrounding the device. “It is incredibly innovative,” says Sarah Aitken, a vascular surgeon at the University of Sydney, but she adds that there are still many unanswered questions about the level of function that people with it can achieve and the ultimate cost of the device. “This kind of research is really challenging to do because it is very expensive” and the surgery involved is very high-risk.
This breakthrough also offers valuable real-world data for medical professionals. Joseph Rogers, a heart-failure cardiologist and president of the Texas Heart Institute in Houston, highlighted that the success of this patient will help researchers better understand how individuals adapt to living with the artificial heart outside of the hospital setting. “They weren’t being constantly monitored by medical teams,” said Rogers, who led the first clinical trial of the BiVACOR device in the United States.
The BiVACOR heart has only been used as a temporary solution in all cases to date, with the ultimate goal of receiving a donor heart. However, some experts believe it could eventually serve as a permanent alternative for patients who are not eligible for transplants due to factors such as age or other medical conditions. This possibility remains to be proven through future clinical trials.
Image credit: BiVACOR