Lab-grown kidney helps test alternative drugs
Drug use is extensive in the intensive care units of many hospitals, and although lifesaving, the practice is fraught with complexity. One notable complication is kidney toxicity, which develops more readily in ICU patients because of the underlying health conditions that enhance risk. The problem affects two out of three patients, according to a study on ICU drug use by Kidney International.
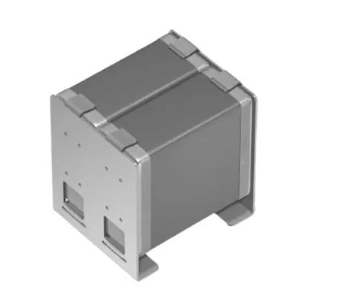
In addressing this challenge, Draper engineers have developed a kidney-on-a-chip—a tiny 3-D structure that mimics features of a full-sized kidney—from human cells.
By reproducing a kidney in a microfluidic device, and creating 96 of those kidneys in a device called PREDICT-96, Draper hopes to give scientists a better model to study the effects of disease and to discover new therapeutics for the kidney and other organs.
Kidneys are one of the most difficult human organs to treat because of their complexity. The primary structural unit of the kidney, called a nephron, is a highly organised tubule under constant exposure to fluid-flow stress from the blood and fluids it filters. Nephron cells receive cues from the extracellular matrix, a network of structural and signaling proteins.
The complexity makes it difficult to build a functional, physiologically relevant organ in the lab, but not impossible, according to Joseph Charest, a Ph.D. in biomedical engineering who helps customers build artificial organ systems to test and refine new drug therapies.
“Given that the kidneys play a major role in how drugs interact with the body, these organs take on a particular relevance for drug R&D,” Charest said. “Nephrotoxity is a major cause of attrition during pre-clinical, clinical and post-approval states in pharmaceutical drug development".
"Even after drug approval, nephrotoxicity resulting from exposure has been estimated to contribute to 19% of all cases of acute kidney injury in critically ill patients. That’s a number we would like to lower.”
A paper detailing the discovery was published in the online issue of the Public Library of Science. Among the findings, Charest and his colleagues demonstrated that Draper’s microfluidic device can be used to reconstruct human kidney physiology and function at the cellular and tissue level and quantify dynamic drug-interaction with kidney tissue in real time.
The platform has the ability to screen new drugs for potential kidney toxicity without the need for animal models, elucidate the mechanism of action of kidney-acting drugs and be scaled to generate clinically-relevant sample sizes and pre-clinical studies with ample statistical power.
The paper was co-written by Else M. Vedula of Draper and José Luis Alonso and M. Amin Arnaout, both of Massachusetts General Hospital and Harvard Medical School.
Draper’s microfluidics platform addresses another common challenge for researchers “and that’s identifying ineffective drugs early in the discovery process,” said David O’Dowd, assistant director of Biomedical Solutions at Draper.
“Used early in the drug discovery process, PREDICT-96 should allow developers to refocus resources on the strong candidates earlier and end unproductive research earlier, minimising losses. What researchers want in a platform is to recreate human physiology in an accurate, reproducible, scalable, high-throughput, cost-effective and predictive format for testing candidate therapies for safety and efficacy. Draper does that with PREDICT-96.”
Draper has modeled liver, kidney and other organs and has partnered with a pharmaceutical company and consumer products company to develop configurations of its PREDICT-96 human organ system. Draper also has collaborated with a university to link organ chips together to predict the effects of potentially toxic chemicals and drugs on the human reproductive system.