Intravenous delivery system for treprostinil
Current guidelines in the United States and Europe recommend treatment with parenteral prostanoids for severe or rapidly progressing pulmonary arterial hypertension (PAH).2-4 However, risks and complexities associated with the current intravenous (IV) and subcutaneous (SC) delivery systems limit the acceptance of parenteral therapy. IV delivery via an indwelling central venous catheter is associated with the risk of serious bloodstream infections (BSI) and unintended catheter dislodgment, which may be fatal.
SC treprostinil delivery is associated with site pain and reactions which can be intolerable. An implantable system for treprostinil not only allows PAH patients to return to normal daily activities without concerns (e.g., bathing without fear of infection, sleeping without worry of dislocating or kinking their catheter), but also reduces the risks of these severe consequences associated with the external delivery systems.
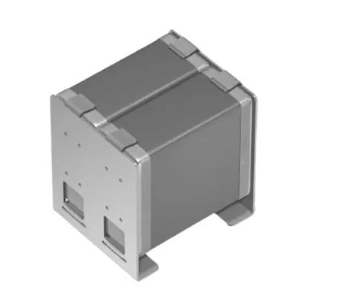
The implantable system for treprostinil, currently under review by the U.S. Food and Drug Administration, consists of the SynchroMed II implantable pump and associated programmer, and a newly developed implantable catheter specially designed for intravenous use. During implant, central venous access is obtained via the cephalic, subclavian, jugular or axillary vein.
The distal tip of the implantable catheter is placed at the superior caval-atrial junction, and the catheter is secured at the venotomy site using sutures on an anchoring sleeve. The proximal length of the catheter is tunneled from the venous access site and connected to the pump in an abdominal subcutaneous pump pocket.
After surgery, the implanted pump is programmed to deliver a priming bolus followed by continuous infusion of treprostinil, and the external IV infusion pump is discontinued.
The implantable pump is programmed and refilled only by trained experienced clinicians. It can be programmed by telemetry to deliver a wide range of therapeutic flow rates, and refilled percutaneously as needed.
The DelIVery for PAH clinical study was conducted at 10 centers in the U.S. to determine the safety of the implantable system for delivery of treprostinil in PAH patients.
The primary endpoint was the rate of catheter-related complications (infections, occlusions, dislocations and mechanical dysfunction) or procedure-related pneumothorax complications using the implantable system compared with an objective performance criterion (OPC) based on published complication rates with external catheters.
Ancillary endpoints included the incidence of adverse events, and changes from baseline in plasma treprostinil levels, 6-minute walk distance (6MWD), New York Heart Association (NYHA) functional class, quality of life (QoL), treatment satisfaction and delivery-system management time.
The primary endpoint was assessed in June 2013, after the accumulation of 22,013 patient days and all patients completed 6-months of follow-up. Results demonstrated a statistically significant reduction in the rate of catheter-related complications using the implanted system versus the OPC (0.27 /1,000 patient-days versus 2.5/1,000 patient-days; p<0.0001).
Six catheter-related complications were observed in 5 patients, including 3 catheter dislocations (2 patients), 1 venous stenosis, 1 mechanical catheter damage and 1 pneumothorax. Although the catheter dislocations resulted in displacement of the catheter from the vasculature, these patients continued to receive treprostinil subcutaneously.
After these dislocations, which occurred early in the trial, additional training was given to implanters, and subsequently there were no catheter dislocations among the 37 remaining implants. No catheter-related BSIs or occlusions have occurred during the study.
Ten additional complications considered related to the procedure and/or system occurred, including 5 events related to the implant procedure (atrial fibrillation, fever, pump pocket infection, urinary retention and Legionella Pneumonia with septic shock); two events related to the pump (pump pocket seromas); and three events related to the refill process (refill reactions).
Refill reactions are attributed to a small amount of drug exiting the refill needle as it is withdrawn from the pump reservoir resulting in local and/or systemic side effects of treprostinil (e.g., pain, erythema and/or swelling near the pump refill site, and flushing, headache, nausea and/or a decrease in blood pressure). There were 3 deaths among the 60 implanted patients. None were adjudicated to be related to the system, procedure or treprostinil.
BSI rates in patients on IV Remodulin reported in the literature range between 0.36 and 1.13 BSIs per 1,000 patient days.5,6 In the DelIVery clinical study there was one BSI (Legionella Pneumonia with septic shock deemed implant related by the study adverse events committee which occurred 3 weeks post implant) at 22,013 patient days, or 0.05/1,000 patient-days of study participation. Using the lowest reported rate of 0.36/1,000 patient days as comparison, the DelIVery study showed a 7-fold reduction of BSI risk.
Efficacy of treprostinil was maintained via the implantable system. Mean changes in 6-minute walk distance (6MWD) and NYHA from baseline to 6 months post implant were small (1.7 ± 21.6% and 0.0 ± 0. 56, respectively). Plasma treprostinil concentrations one week post-implant highly correlated with baseline concentrations (r=0.91, p<0.0001).
The 60 subjects rated the treatment overall as good (7%), very good (30%), or excellent (63%) 6 weeks post-implant via the Functional Assessment of Chronic Illness Therapy Treatment Satisfaction questionnaire (FACIT-TS-G).
The mean delivery-system management time decreased significantly from 2.5±1.7 hours/week pre-implant to 0.6±0.8 hours/week at 6 months (p<0.0001). The average refill interval in this study was 47.2 days (range, 19.5–94.3 days) versus every 2 to 3 days with the external systems.